Our Story
I saw a 57-year-old Caucasian female with a past medical history of diabetes, hypertension, hyper cholesterol and coronary artery disease. Apart from taking a history, doing a physical examination planning assessment and plan, I always ask this question, “What else do you want to know about diabetes?” Diabetes is a complex disease and if I ask, “Do you have questions?” Most of the time my patients’ answer is nothing. If I ask do you know about diabetes, their answer is always affirmative as they know everything about diabetes. I think either patient knows everything or know nothing. Asking a closed-ended question usually ends the communication with the patient and health caregiver goes to the next patient room. After the encounter with the patient, usually a medical assistant, or a nurse prints out diabetic education material which some patients leave in their cars, others throw in the trash or put in a shredder. Giving a pamphlet and checking the box to appease insurance companies is considered patient education. Can we change habits by just handing a pamphlet?
How did the idea to Flip the Healthcare occurred?
I coach USMLE Step 2 Clinical Skills and have portrayed as a standardized patient for medical students. Young medical minds have taught me how to become a coach and a standardized patient and this practice have helped me in my real-life patient scenarios. I have wondered about health literacy and how should medical students ask questions from me when I am in the workshop with them. I have experimented with many questions asking techniques and discovered a non-threatening way to ask questions is by telling the stories of other patients. However, time being a big constraint, storytelling is next to impossible. I have adopted Lisa Bernstein’s question asking technique— “Many people dealing with diabetes want to know more about complications associated with the disease. Patients are not aware of what to ask, why to ask and how to ask as the medical knowledge is complex. Even as physicians, we forget medical knowledge and must take CME’s, do MOC exams, and recertify for board exams. On occasions, the Utilization Review team has to remind us about ICD 10 coding and mandates. If we as health care providers forget, can we expect lay people to remember the complex medical jargon in just 15 minutes to 30 minutes of the office visits? Coaching medical students and becoming a standardized patient has taught me how to teach real-life patients. As a standardized patient, I increase the difficulty level of the clinical scenario according to the acumen of the medical students and this is where I use the Vital Checklist to portray clinical cases. Sometimes I act as a stubborn patient and on other occasions, I am an angry patient. On occasions, I tell my students to explain about the HbA1C in a layman language and on another instant, I will see if they are asking me about the blood sugar logbook. To teach medical students, I had to devise a checklist of the diabetic complications so as they could explain and communicate easily in the exam. In USMLE Step 2 CS exam, medical students don’t have models or posters and they must memorize symptoms, signs, assessment, and plan. If medical students, our future doctors, memorize the complications of diabetes in the formative years of becoming doctors, they will have an easier time in coaching real-life patients in the future. (iCrush) Diabetes Vital Checklist was developed for medical students but I used for my diabetic patients and everybody loved it. This was the AHA moment for me as I thought of developing a dedicated portal for diabetes where patients can download the (iCrush) Diabetes Vital Checklist in their own native language and be ready to ask questions from their doctors. Giving a patient (iCrush) Diabetes tool may help to flip the healthcare, an idea adopted from the Khan’s Academy Flip the Classroom. Proactive patient education is a key to improve the patient experience. Therefore, I have developed L.E.A.N. Patient Experience and this L.E.A.N not only represents Lean Health Care but also represents Listen >> Educate >> Activate >> eNgage. My work heavily depends on checklists and these checklists are not there to tell what to do but they are gentle reminders of what we should not forget.
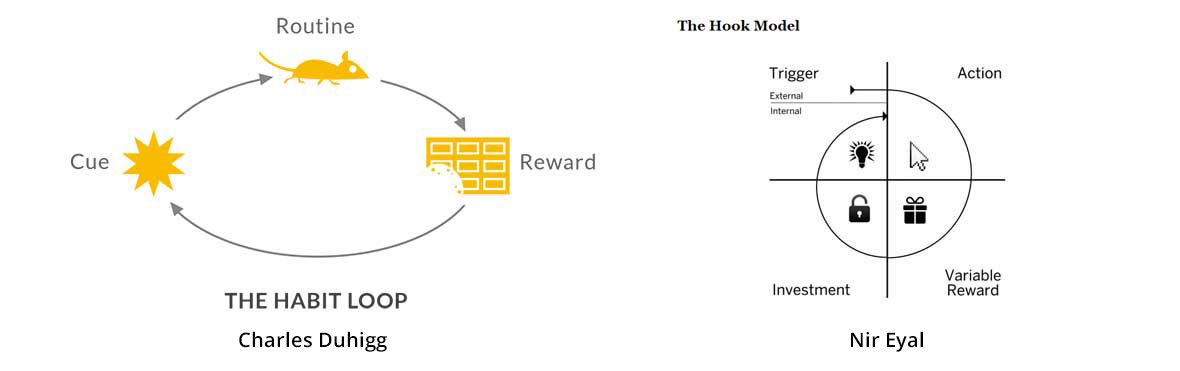
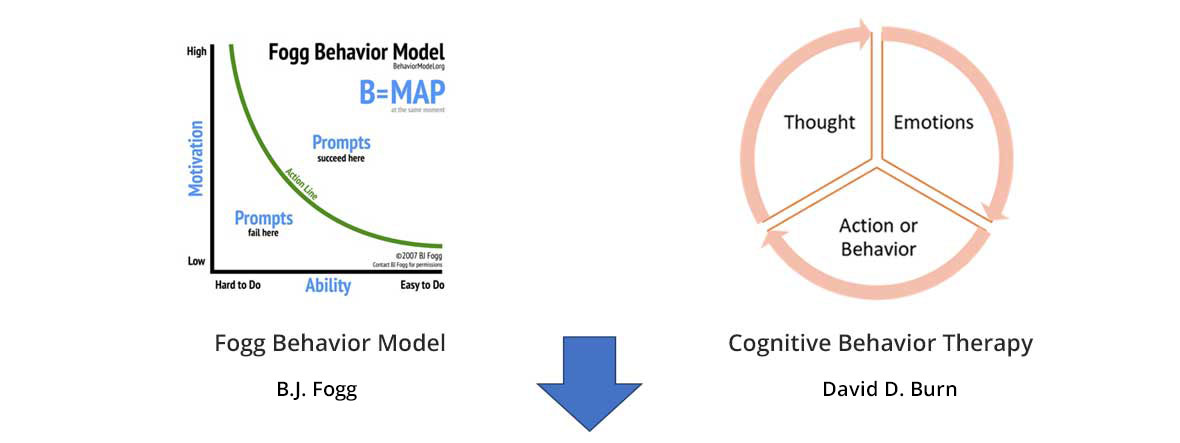
Changing Habits: L.E.A.N Patient ExperienceDr. Atul Gawande has shown how safe surgery checklist dropped the mortality and morbidity and this was the idea which has encouraged me to implement my idea of (iCrush) Diabetes. To make the checklist memorable, I needed to chunk the checklist and include the actionable words, and this is how I came up with my checklists. I am indebted to Charles Duhigg (The Power of Habit), Nir Eyal (Hooked), B.J. Fogg (TinyHabits.com), David D. Burns (Feeling Good and Cognitive Behavior Therapy) whose work I have combined to make one Benzene Loop which I also call L.E.A.N. Patient Experience.
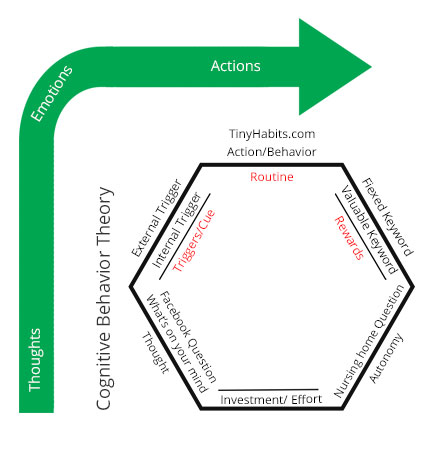
Benzene Loop or LEAN Patient Experience.
Disclaimer: I have derived this LEAN Patient Experience model from the work of great philosophers and psychologists—Charles Duhigg, Nir Eyal, B.J.Fogg and David D. Burns. I don’t claim this to be my work. I have read their books and combined to make one model and use this model to make happy patients.
L.E.A.N. Patient Experience
-
External Trigger:
- Doctor‘s visit
- High Blood Sugar
- Family member encouraging taking care of diabetes
- advertisement about the diabetes
- Email notifications
Internal Trigger: Stroke, Eye damage, Kidney damage, Heart Attack, Amputation. Just giving a pamphlet about the side effects and complications cannot create a strong internal emotion. Giving a structured checklist (iCrush) Diabetes, may provide more recall of the complications
- I: Infections, Ulcers on the foot, cellulitis or Amputations
- C: Cholesterol and atherosclerosis
- R: Records of the blood sugar and maintaining your food diary
- U: Urine proteins and microalbuminuria; Diabetic Nephropathy; Chronic Kidney disease; Kidney Failure, End-stage renal disease or dialysis
- S: Stroke, paralysis
- H: Heart attack, coronary artery disease
- D: Depression or dementia (forgetfulness)
- I: Impotence or erectile dysfunction
- A: A1C or long-term sugar evaluation
- B: Blood pressure log book; high blood pressure may cause stiffness in the heart
- E: Eyes or diabetic retinopathy, cataracts
- T: Tingling in the legs or diabetic neuropathy
- E: Ears or sensorineural hearing loss
- S: Stomach or gastroparesis
-
Behavior, Action or Routine:
- BJ Fogg’s behavior model focusses on the ability first and then on the motivation. Change tiny habits like learning a symptom and complications checklist rather than exploring the internet for the symptoms of diabetes.
- (iCrush) Diabetes Vital Checklist patient education tool is the starting point.
- Top of mind awareness about diabetes with various touch points—web apps, apps, t-shirts, flash cards, books.
- Instead of symptom checker, we provide chunked symptom checklist for an easier memory and recall.
- An easy to share checklist with family and friends
What problem is (iCrush) Diabetes trying to solve?
Diabetes is a complex disease and if it is difficult for health caregivers to remember complications then it may be difficult for patients to remember each detail. Some patients search the internet to learn about the symptoms but rather than checking symptoms on symptom checker, we need to encourage patients to use symptom checklist or Vital Checklist.
Proactively asking questions about diabetes and preventing the complications.
- Rewards of the Tribe Sharing (iCrush) Diabetes may make you feel accepted and important. Most importantly saving a life of a diabetic individual by teaching complications of diabetes gives a good feeling. Sharing (iCrush) Diabetes on Facebook is the powerful social validation.
- Rewards of the Hunt Sharing a free (iCrush) Diabetes checklist with other patients, family, and friends. Sharing is caring
- Rewards of the Self Mastery and completion on (iCrush) Diabetes
The sense of achievement when patients feel they are in the control of their disease. This can happen only if they know about diabetes.
Investment:Learning about diabetes is more comfortable with the checklist, and therefore patients may adopt it easily. Minimal time and maximal output.
Thoughts:Thoughts that come to the mind should trigger the emotion and this leads to the action.
What is depression? Depression is the repressed anger or bottle-up frustration which leads to negative emotions leading to inaction. In cognitive behavior therapy, we have many thought distortions or zombies which overpower your thought process. Thinking on the paper and writing all the negative thoughts and changing your habits by tackling the smallest elements first may help to overcome negativity. Knowledge about diabetes and its complications can help the patients to overcome the negative thoughts. It is essential to focus on the ability rather than motivating to take care of themselves.
Thoughts >> Emotions >> Action = Cognitive Behavior Theory
Cognitive Behavior Therapy + The Power of Habit Loop + Tiny Habits + Hooked Model + Autonomy= L.E.A.N. Patient Experience Model
I saw a 57-year-old Caucasian female with a past medical history of diabetes, hypertension, hyper cholesterol and coronary artery disease. Apart from taking a history, doing a physical examination planning assessment and plan, I always ask this question, “What else do you want to know about diabetes?” Diabetes is a complex disease and if I ask, “Do you have questions?” Most of the time my patients’ answer is nothing. If I ask do you know about diabetes, their answer is always affirmative as they know everything about diabetes. I think either patient knows everything or knows nothing. Asking a closed-ended question usually ends the communication with the patient and health caregiver goes to the next patient room. After the encounter with the patient, usually a medical assistant, or a nurse prints out diabetic education material which some patients leave in their cars, others throw in the trash or put in a shredder. Giving a pamphlet and checking the box to appease insurance companies is considered patient education. Can we change habits by just handing a pamphlet?
Read More...
The checklists, text, graphics, images, videos and other material contained in the videos and Vital Checklist Website ("Content") are for informational purposes only. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read or heard on the Vital Checklist website, its videos or other concepts.
In accordance to the HIPAA regulation, a duly informed consent was taken from the real-life patients, students, caregivers or other individuals appearing in the informational videos presented on this website.
If you think you may have a medical emergency, call your doctor or 911 immediately. Vital Checklist website and videos do not recommend or endorse any specific tests, physicians, products, procedures, opinions, or other information that may be mentioned on the Site. Reliance on any information provided by Vital Checklist website/videos, Vital Checklist employees, others appearing on the Site at the invitation of Vital Checklist, or other visitors to the Site is solely at your own risk.
The Site may contain health or medical-related materials that are sexually explicit. If you find these materials offensive, you may not want to use our Site. The Site and the Content are provided on an "as is" basis.

